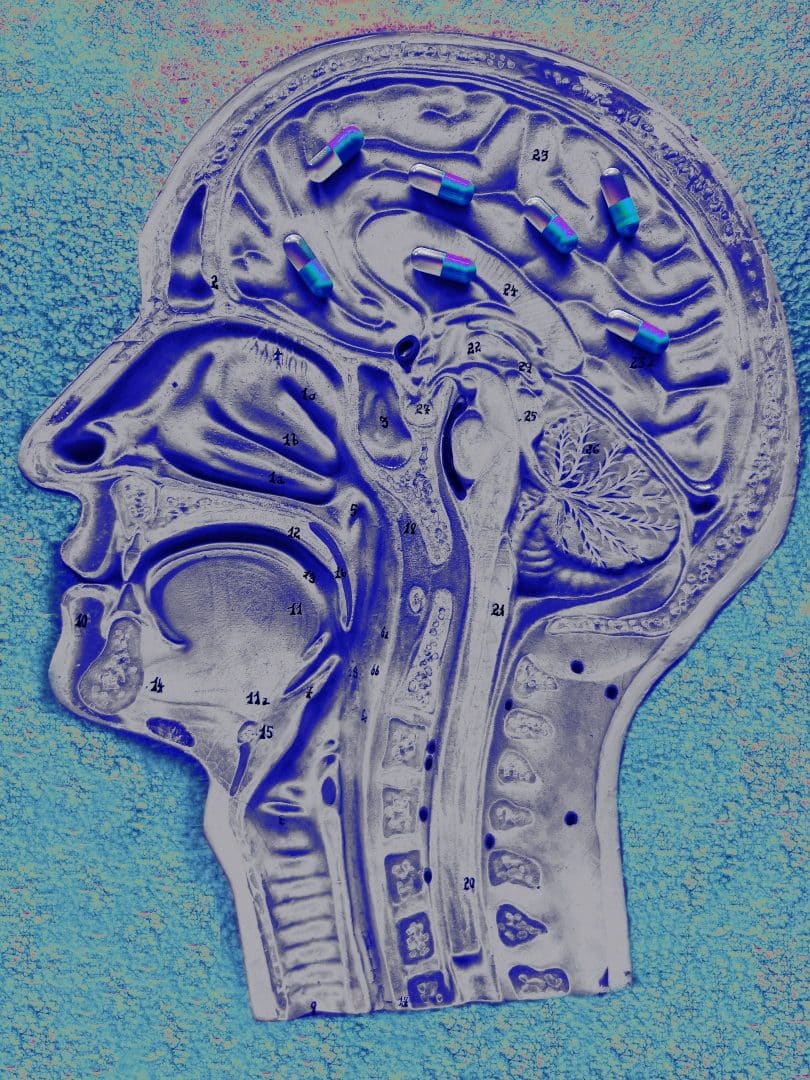
MDMA is one of two hallucinogenic compounds that is likely to get an approval soon in the US. Mainly because of its benefits for PTSD patients. How does it do what it does? A recent study using brain imaging helps explain how MDMA might help lessen the fear response in people with PTSD. Read on for details.
Recent trial into MDMA for PTSD
In the introduction to their study, Altered brain activity and functional connectivity after MDMA-assisted therapy for post-traumatic stress disorder, researchers point out that “MDMA is hypothesized to facilitate the therapeutic process, in part, by decreasing fear response during fear memory processing while increasing extinction learning.” PTSD patients are known for dealing with excessive fear responses.
The purpose of the current study was to analyze the brain’s activity and connectivity using fMRI technology, before and after MDMA treatment. Scans were done during rest (neutral) and during an autobiographical memory response (trauma) before the administration of MDMA, and two months after. Nine veterans and first-responders were used for the study; all with chronic PTSD for at least six months.
The fMRI component allows investigators to see “changes in regional blood oxygenation over time and is thus used as a proxy for fluctuating neuronal activity.” The researchers also explain how the fMRI data can allow functional connectivity to “be assessed to infer interaction between two or more brain regions’ activity over time.” fMRI scans show metabolic activity, whereas a standard MRI creates a picture of internal structures. They are performed the same way.
They go on to say that “PTSD patients have shown altered functioning of the precuneus, posterior cingulate cortex (PCC), anterior cingulate cortex (ACC), insula, prefrontal and frontoparietal regions, as well as the hippocampus and amygdala.” These locations relate to “augmented recruitment of brain regions involved in self-referential processing, salient autobiographical memory, and fear and emotion.”
The study is a sub-study of a larger clinical trial; meaning the participants were already involved in a study, from which this study takes data. All participants agreed to be a part of this study as well. The larger study is a “Phase 2 randomized, double-blind, dose-response trial of MDMA-AT in veterans and first responders with severe and chronic PTSD.” Those that signed off on the sub-study, agreed to have the fMRI scans done as well.
Those that participated in the fMRI study, worked with investigators to create an auditory script about their traumatic event, as well one about an ordinary experience (typical morning routine). Each recording was six minutes, and made by the participant reading their own script. This scripts were to assess symptom provocation. All participants had an image done at baseline before the MDMA treatment, and then two-months after the final session.
Study results
Though researchers had thought MDMA-AT would increase functional connectivity in the amygdala-hippocampus during the resting state, they only found this to be the case on the left side of each. They also found lessened activation contrast in the cuneus, after treatment with MDMA.
They detail how the amount a person recovered after the MDMA treatment, was correlated to change in four different ways during autobiographical memory recall. These relate to the functional connectivity in four different areas.
They state that “Amygdala—insular functional connectivity is reliably implicated in PTSD and anxiety, and both regions are impacted by MDMA administration.” And that “These findings compliment previous research indicating that amygdala, hippocampus, and insula functional connectivity is a potential target of MDMA-AT, and highlights other regions of interest related to memory processes.”
The investigators measured and compared the whole brain’s activation by the scripts, both at the baseline, and two months after MDMA treatment. They found that before the MDMA, there were larger levels of activation for the traumatic script than the neutral one, in four separate areas of the brain. Post-MDMA treatments, the magnitude of difference between the activation levels, was much smaller.
Researchers also looked at functional connectivity between 18 different brain regions of interest during the fMRI, comparing the traumatic and neutral experiences. According to their research, none showed significant change after corrections for multiple comparisons. However, before the corrections, there was significant modification in the right amygdala to left caudal ACC.
When researchers correlated individual changes from before and after MDMA treatment of these functional connections, with individual reductions in CAPS-IV scores (evaluation test for PTSD symptoms), “Most correlations were positive, meaning that larger reductions in connectivity from pre- to post-therapy corresponded to larger improvements in PTSD symptoms.”
They found the four most significant changes following comparison corrections, were: left amygdala and left PCC, left amygdala and right PCC, left amygdala and left insula, and left isthmus cingulate and left hippocampal tail.
Researchers conclude, “We also provide preliminary evidence that MDMA-AT alters brain response during symptom provocation in regions associated with fear response, anxiety, self-referential processing, and salient autobiographical memory, and are commonly found to be hyperactive in PTSD patients.”
What is PTSD?
Post-traumatic stress disorder is a psychiatric disorder, which is diagnosed subjectively, but based on criteria in the DSM-V. All psychiatric disorders are diagnosed in this way, as there is no specific test to define these issues. A medical diagnosis is a diagnosis based on information verified through some kind of test or investigation. Unfortunately, psychiatric disorders don’t have this, and therefore are made at the discretion of the individual doctor.
I like to mention this, because it does play into the idea that doctors often disagree, or have their own opinions that they go by. Because of this, any patient can receive multiple different diagnoses for the same set of symptoms. Which also means, when looking at psychiatric disorders, since no testing is available, they are based 100% on symptoms and observable behavior.
In the case of PTSD, this relates to symptoms and behaviors experienced after a traumatic event, whether it was experienced directly or indirectly (witnessed, heard about…) Though there are countless scenarios that can bring on PTSD symptoms, some of the more common ones include: physical attacks, being the target of bullying or psychological abuse, being a part of or witnessing the atrocities of war, and natural disasters. PTSD can be quite debilitating in some sufferers, making it difficult to perform regular life functions.
In WWI this was called ‘shell shock.’ In WWII it was known as ‘battle fatigue.’ It is associated with the idea of re-experiencing an intense trauma, after the incident occurred. This can happen at different frequencies for different sufferers, and is often set off by a trigger; something that works to remind the person of this past trauma. Sufferers might experience nightmares or flashbacks, and feelings of sadness, fear, anger, detachment, and estrangement.
Psychiatry.com says that about 3.5% of American adults have PTSD, and that 1/11 will experience it at some point during life. Women outnumber men with this condition at a rate of 2:1. In America, the largest groups to suffer from PTSD are Latinos, Native American, and African Americans. This is likely from the extreme violence, intolerance, and general negative treatment suffered by these populations throughout American history.
Not only is MDMA undergoing testing now for PTSD, it was a point of research in the past, following Alexander Shulgin’s new way to formulate it in the 1970s. Beyond PTSD, its also under investigation for some sexual disorders; particularly related to sex drive. The company MAPS was given a Breakthrough Therapy designation for its MDMA drug currently in trials for PTSD. And the state of Colorado already legalized the drug pre-emptively, which goes into effect upon a federal legalization. All this is to say that MDMA is definitely getting a lot of attention these days; for PTSD and beyond.
Conclusion
Most studies thus far with hallucinogens (and other drugs) involve self-report of symptoms on different measures, or observation of behaviors; as the main ways to assess therapeutic change. The interesting thing about this study is that it uses actual brain imaging to understand how the brain changes and reacts differently, after use of MDMA. Perhaps we will see more intensive investigations like this in the future. For now, we have a little more to go on regarding the use of MDMA to treat PTSD symptoms.
Hello and welcome! We appreciate you joining us at Cannadelics.com; an independent publication investigating different topics in the cannabis and hallucinogen industries. Head our way whenever you get the chance to stay up on current stories; and subscribe to the Cannadelics Weekly Newsletter, to ensure you get all updates on time.